As the world marks Malaria Day today, Nigerian families are still battling the scourge, with a whopping N1.156 trillion spent on treatments annually.
Although malaria is preventable, it remains a major public health challenge in Nigeria, placing a significant financial burden on families who frequently grapple with the cost of treatment.
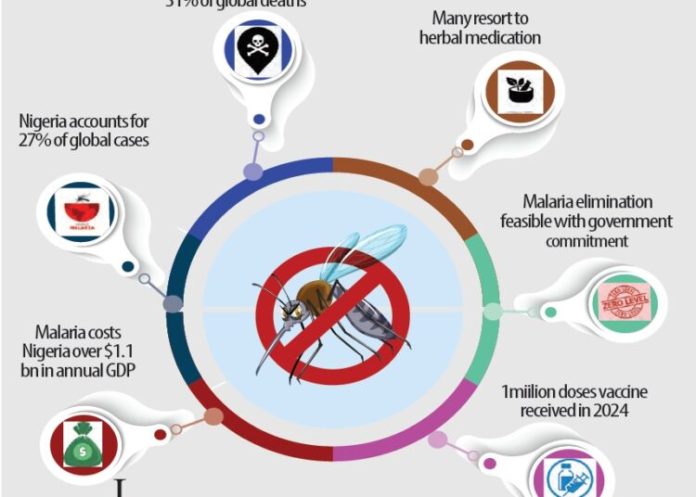
According to the World Health Organisation’s (WHO) 2022 report, Nigeria recorded an estimated 68 million malaria cases and 194,000 deaths in 2021, making it the country with the highest malaria burden globally, accounting for nearly 27 per cent of all cases worldwide.
LEADERSHIP’s checks revealed that treating a single case of uncomplicated malaria in public hospitals, including consultation, diagnosis, and medication, costs about N17,000. This amounts to roughly N1.156 trillion for all the cases, but the actual figure is likely much higher, as many cases are complicated and can cost up to three times more than an uncomplicated case.
As the world marks World Malaria Day, WHO has reiterated that malaria remains a life-threatening disease, particularly in tropical regions, despite being both preventable and curable.
World Malaria Day 2025, with the theme “Malaria Ends With Us: Reinvest, Reimagine, Reignite,” emphasises the need for renewed commitment, innovation, and investment in the fight against malaria.
Therefore, health sector stakeholders have called for increased investment in malaria to achieve elimination targets and zero deaths.
The president of the Nigerian Association of Resident Doctors (NARD), Dr. Osundara Tope Zenith, stressed the need for stronger political will and increased government funding to eliminate malaria.
He described the disease as a significant public health challenge with devastating effects, especially on children under five and pregnant women.
Dr. Zenith underlined the heavy burden of malaria across nearly all parts of the country, noting that the disease continues to impact health outcomes negatively and remains a significant concern for both the government and the Ministry of Health.
“Malaria is endemic in this country. The burden is enormous, and while we have made progress in handling treatment, eliminating malaria will require much more,” he said.
He highlighted multiple factors influencing malaria transmission, including rainfall, climate conditions, and even hidden reservoirs of the malaria parasite in animals and humans.
According to him, some parasite strains can remain dormant in the liver for months, leading to relapses even after successful treatment.
Dr. Zenith also raised concerns about growing resistance to malarial drugs and insecticide-treated nets that have long been central to prevention strategies.
“Some malaria parasites are building resistance, not only to drugs but also to the insecticides used in treated nets. This complicates the fight,” he said.
He added that beyond medical intervention, poor sanitation and environmental conditions in many communities, such as stagnant water and overgrown vegetation, continue to provide breeding grounds for mosquitoes, further hindering eradication efforts.
While acknowledging that the goal of eliminating malaria is not entirely unrealistic, he cautioned that it is a challenging target that can only be achieved through sustained political commitment and a multifaceted approach.
The NARD president told LEADERSHIP that the government’s level of investment in malaria control is inadequate, and is heavily reliant on international donors.
“We still depend on funding from institutions like the World Bank, the African Development Bank, and the Global Fund. Government contribution has not been enough,” he said.
To achieve meaningful progress, he urged increased domestic funding, improved public awareness, continuous development of new treatments and insecticides, and a stronger emphasis on environmental sanitation.
“Eliminating malaria is possible, but we need persistent commitment and a stronger, well-coordinated national effort to make that dream a reality,” he said.
Also, a consultant pathologist at the Lagos State University College of Medicine and Teaching Hospital, Professor Francis Faduyile, called for a comprehensive and preventive approach to tackling deaths caused by the disease, particularly among children.
Professor Faduyile emphasised the urgent need for increased public health education, improved healthcare access, and effective universal health coverage implementation to curb malaria-related mortality.
“If anybody wants to fight against death from malaria, which primarily affects children, there are critical things that must be in place: first, parents need proper education on how to treat and prevent malaria in their children; second, they must have access to healthcare systems where adequate management can occur; third, economic empowerment is vital so families can afford treatments,” he said.
Prof. Faduyile, a former president of the Nigerian Medical Association (NMA), noted that eliminating malaria deaths would remain elusive unless these three pillars—education, accessibility, and affordability—are addressed simultaneously.
According to him, functional primary healthcare centres and a robust health insurance system are essential to universal health coverage that could drastically reduce deaths from communicable diseases, including malaria.
Reflecting on past efforts to combat the disease, Faduyile said preventive strategies such as prophylactics, vector control, and various public campaigns have had limited success because they have not been widely embraced or effectively coordinated.
“We need widespread health education to teach people how to control the mosquito population, the vector responsible for malaria transmission. Mosquitoes thrive in dirty environments with stagnant water. Until we address environmental cleanliness and get everyone involved in preventive practices, we can’t truly aim for zero malaria deaths,” he said.
Prof. Faduyile stressed that prevention remains the most cost-effective strategy in the fight against malaria and other infectious diseases.
“It is far better and cheaper to prevent than to cure. Let’s focus on mopping up the causes of malaria transmission and back it up with universal health coverage. Only then can we see a meaningful reduction in malaria-related deaths,” he said.
In the same vein, a senior lecturer and head of medical microbiology and parasitology at the University of Port Harcourt Teaching Hospital, Dr. Mary Alex-Wele underscored the need for a more holistic approach to prevention beyond mosquito nets.
“We live in a malaria-endemic environment. The mosquitoes are here with us and carry the parasite,” Dr. Alex-Wele said, highlighting the daily persistent risk residents face.
While acknowledging the importance of mosquito nets, she stressed that environmental cleanliness plays a vital role in reducing malaria transmission.
“Certain environments encourage the breeding of mosquitoes, like dirty environments, bushy areas, and places with stagnant water. If we take care of these, we will reduce the burden of mosquitoes around us,” she explained.
Dr. Alex-Wele also recommended using insect repellents and sprays as part of an integrated malaria prevention strategy and prophylaxis for high-risk groups.
“Certain people, like pregnant women, travellers from non-endemic regions, and individuals with conditions such as sickle cell disorder, may be placed on prophylaxis by a doctor,” she noted.
According to her, healthcare providers assess and determine the need for such preventive treatment on a case-by-case basis.
According to the WHO, malaria is caused by a parasite and transmitted to humans through the bites of infected female Anopheles mosquitoes. Unlike the flu or COVID-19, malaria does not spread from person to person. However, in rare cases, it can be transmitted through blood transfusion or the use of contaminated needles.
WHO said the early symptoms of malaria include fever, chills, and headache, which typically appear 10 to 15 days after being bitten. These signs can be easily mistaken for other feverish illnesses, making early diagnosis and testing crucial.
If left untreated, infections, particularly Plasmodium falciparum malaria, can become severe and even fatal within 24 hours.
Severe malaria symptoms include extreme fatigue, confusion, difficulty breathing, seizures, dark or bloody urine, jaundice, and abnormal bleeding. Vulnerable groups such as infants, children under five, pregnant women and girls, travellers, and individuals with HIV or AIDS are at higher risk of experiencing severe illness or death, the global health body explained.
WHO said five Plasmodium species cause malaria in humans globally, with P. falciparum and P. vivax posing the most significant threat. P. falciparum is the most dangerous and common in sub-Saharan Africa, while P. Vivax dominates in parts of Asia and Latin America.
Malaria can be prevented through insecticide-treated bed nets, indoor spraying, and antimalarial medications. WHO emphasised that timely treatment can effectively stop mild cases from worsening.
“Getting tested and treated early is the best way to save lives,” WHO said, urging continued investment in prevention, treatment, and education.
Meanwhile, our correspondent visited one of the densely populated slums in the Federal Capital Territory (FCT). The slum, located in Jikwoyi, revealed a grim reality where hundreds of families, especially children, live in squalid conditions by gutters filled with stagnant water and refuse.
Our correspondent described the scene as heartbreaking, with children playing barefoot in dirty surroundings, oblivious of the health risks.
Many households used shared public bathrooms, with wastewater flowing directly into the streets or nearby gutters. Broken pipes and faulty soakaways have turned compounds into pools of dirty water, seeping up to doorsteps.
One of the residents, Mama Ozioma, shared her struggles.
“I’m not happy living here, but we don’t have a choice. Rent in better areas is too high for me and my husband,” she said.
The impact of these poor living conditions is evident in the health of residents, particularly children.
“Malaria is constant in this place,” she lamented. “My children fall sick often, and I can’t even take them to the hospital. I used to buy drugs from a nearby chemist, but now the medicine that was N500 is N1,500. I can’t afford it anymore.”
Mama Ozioma and many like her have turned to traditional remedies to cope.
“We now use agbo. I boil mango, orange, and pawpaw leaves, and we drink them. Only when it gets worse do I buy drugs or go to a nurse,” she said, noting that a visit to the nurse can cost as much as N10,000 per child, including tests and treatment.
When asked about preventive measures like mosquito nets, she explained, “One mosquito net cannot cover five children. Even when we had one, the children tore it while playing.”
The dire situation in Jikwoyi mirrors the broader challenges of urban poverty, limited access to healthcare, and the rising cost of essential medicines.
As Nigeria rolls out the malaria vaccine in
selected states, residents of underserved communities in the FCT continue to rely on local herbs and hope because that’s all they can afford.
LEADERSHIP investigation also revealed that consultation fees at most general hospitals in the FCT are pegged at N2,200, while a malaria test costs N2,000.
A physician at one of the general hospitals spoke anonymously and told our correspondent that malaria treatment now typically includes both injections and tablets. When combined with the cost of consultation and diagnosis, the total expense for treating malaria can amount to approximately N17,000.
Meanwhile, the federal government has declared malaria not just a health concern but an economic and developmental emergency, urging swift and coordinated action to eliminate the disease.
To this end, the ministry inaugurated an Advisory on Malaria Elimination in Nigeria (AMEN) in 2024.
Minister of Health and Social Welfare Prof. Ali Pate described the launch of AMEN as a bold move to confront a “wicked problem” that has long undermined Nigeria’s health and economic progress.
“Malaria continues to take an unacceptable toll on our country. Nigeria accounts for 27 per cent of global malaria cases and 31 per cent of malaria deaths. In 2022 alone, over 180,000 children under five died from this preventable disease,” he said.
Prof. Pate also underscored the economic burden of malaria, estimating an annual loss of over $1.1 billion in GDP.
“This is more than a health crisis. It drains productivity, deepens poverty, and increases out-of-pocket healthcare costs,” he added.
The health minister called for grassroots involvement, urging traditional and religious leaders to drive behavioural change by promoting insecticide-treated nets, chemoprevention, and vaccines.
Nigeria received about one million doses of malaria vaccine in 2024, targeting children in high-burden areas. The vaccines were deployed in Kebbi and Bayelsa states, which were identified as having some of the highest malaria burdens in Nigeria.
The executive director of the National Primary Health Care Development Agency (NPHCDA), Dr Muyi Aina, said as part of a phased rollout, the agency vaccinated 101,158 children in the two states, noting that the initiative was integrated into existing immunisation schedules and outreach programmes to enhance reach and effectiveness.
He acknowledged that vaccine supply constraints and the novelty of the rollout strategy presented challenges.
“We needed to learn from this new experience, even as we managed limited supplies,” he added.
LEADERSHIP